When we talk about clearing your chest we are talking about removing excess sputum.
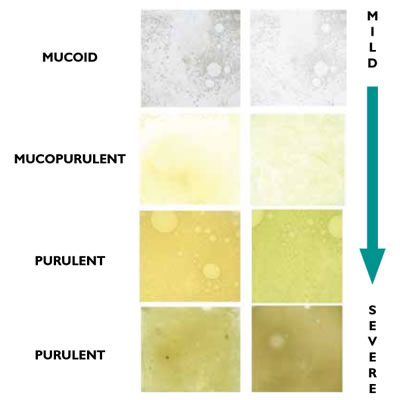
Sputum chart
Sputum classification
Sputum may be clear or white and frothy (mucoid).
Sputum which is slightly thicker and cloudy or opaque (mucopurulent).
If you have an infection you may see the colour of your sputum getting darker with either a yellow or green tinge. (purulent) This can be a sign to get early advice and medication from your GP or practice nurse.
If the sputum is darker green (severe purulent) it may also start to become thicker and more difficult to cough up in order to clear your airways. This can be caused by a virus or bacteria.
Mucous plugs which can block the small airways can occur at any stage where mucous is becoming thicker and stickier.













