This is a peak flow meter and I’m going to show you how to use it.
Slide the pointer down to the bottom of the scale.
Lightly hold the meter on its edge in front of you, with the scale away from your hand.
Take as deep a breath in as you can.
Hold your breath. Place the mouthpiece well into your mouth and seal your lips firmly around it.
Blow as hard and as fast as you can for a second or more, being careful not to block the mouthpiece with your tongue or your teeth.
And I’m now going to show you how to do it.
INHALES
EXHALES
Your peak flow reading is show on the scale against the pointer.
Make a note of the reading and slide the pointer back to the bottom of the scale.
Blow in 3 times and make a note of the reading after each time, and then compare the highest score with your action plan.
You will soon get to know your own normal readings.
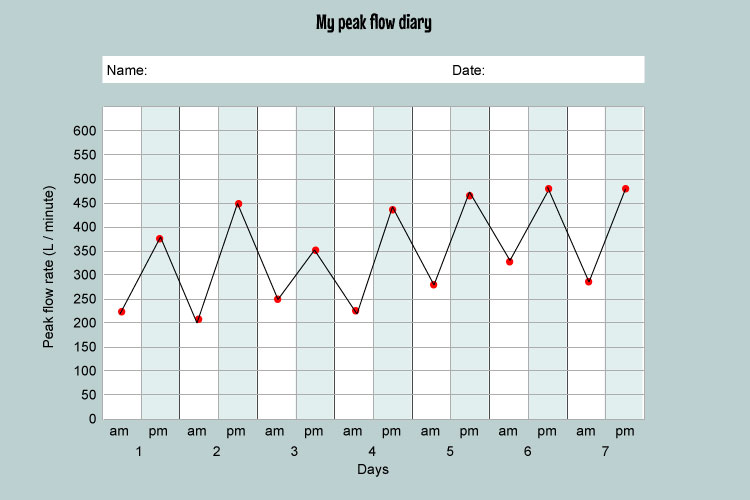
You should take the peak flow reading twice a day, morning and evening.
If you become unwell, one of the first signs you might notice is a change in your peak flow reading.
If there are big differences between your morning and evening readings, or if you start to wake at night with a cough or a wheeze, this could be a sign that your asthma is worsening and you should seek medical advice.