Young girl in a hospital bed
- Occasionally your child may be admitted to hospital if they are very wheezy, their oxygen levels are low or they need help with their feeding.
- The nurses will make regular observations of your child’s temperature, heart rate, breathing and oxygen levels.
- Your child may be given extra oxygen if their levels of oxygen are low. This can be given by a mask or small tubes called a cannula that fit just inside the nose.
- Your child may be given a short course of oral steroids to reduce any inflammation or redness in their airways, usually for 3 or 5 days.
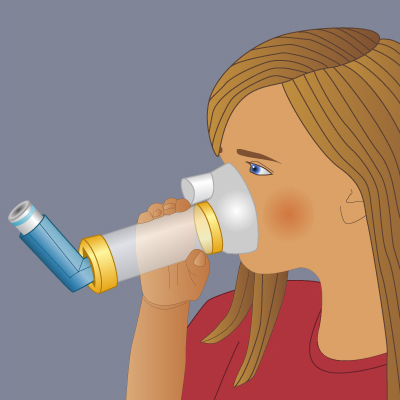
The nurses will give any inhalers that have been prescribed and monitor their effect. - As a parent you should be given instructions on how to give your child their inhalers correctly or how to supervise them while they are taking them by themselves. Medicine can only work if it is taken properly.
- If you have questions about your child’s asthma or how to help them get back to normal activity such as school or exercise speak to the hospital staff.
You could ask for an individual child asthma plan and leaflets which you can take home or go through with the staff.
Check list for parents at time of discharge
- Are you sure you know how to supervise your child taking their inhaler properly?
- Has someone given you enough information about any new drugs your child has been given?
- Are you confident in your abilities to manage a severe attack? When you should get help in the future?
- Does anyone need to be informed about any changes to your child’s care, e.g. school, child minder, after school club or other family members?