There are different types of spacer.
It is better to use a small volume spacer than no spacer at all.
Using the small spacer with the Metered Dose Inhaler or “puffer” inhaler gets about 60% of the inhaled medicine into the child’s lungs.
Here are some of the percentages showing how much (or how little) of the inhaled medicine you get using different devices
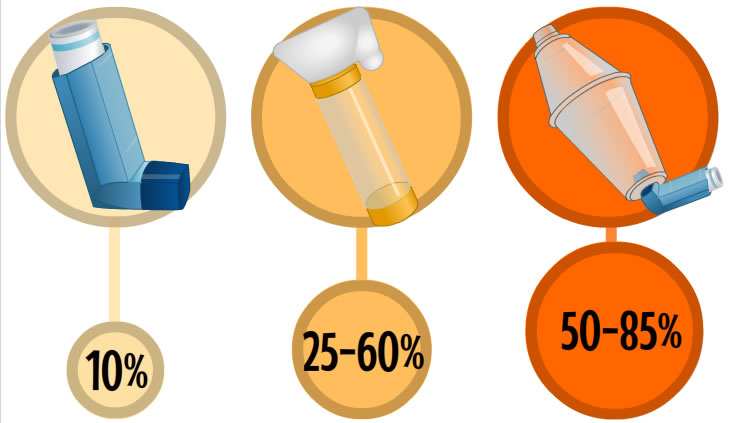
Percentage of inhaled medicines, depending on device used.
You will see that with both spacers you get up to 6o or 85% of the medicine into your child’s lungs. that means that you lose approx 15 – 40% of the medicine from every puff. This is normal, so don’t worry if you see some vapour coming out of the end of the spacer or inhaler.
Large volume spacer
Aerochamber
A spacer is a chamber where the medicine is held. Only use one dose of medicine at a time. The inhaler is fitted to it and the number of “puffs” go in to the spacer so it can be taken during several breaths rather than in one big breath. You may need to repeat the inhaler technique again for more than one dose.
There are different sized spacers for children of different age groups.
Once the medication is in the spacer it needs to be breathed in fairly quickly, within a minute or so. If you think your child hasn’t had their full dose in that time, stop and try again.
One dose of medicine from the inhaler should be used at a time in the spacer to ensure that the correct dose is delivered. If more than one dose is fired into the spacer at the same time, the full dose may not be delivered.
The most effective way to get inhaled medicine into a child’s lungs is to use a Metered Dose Inhaler (MDI) or “puffer” with a spacer. This gets about 80% of the inhaled medicine into the child’s lungs.
For very young children get them used to handling the inhaler and spacer.
Make sure the child is calm and comfortable on your knee or for babies lying down is best.
Try to make it a fun experience. Some parents sing nursery rhymes rather than counting slowly to ten. Practice on their favourite toy to get them used to the inhaler and spacer.
If the child is very distressed and crying they will not be able to breathe deeply to get the medicine in to the lungs. Stop and try again when they are calmer. If this keeps happening ask for help from your asthma nurse specialist or pharmacist.
Video from Itchy Sneezy Wheezy.
Inhaler technique can be hard to get right even for a co-operative, well coordinated adult who is motivated and understands why they need to take an inhaler. They can be very challenging to give an unco-operative, sick or distressed child who might not understand what the inhaler is for. However it is not impossible. It will take practice, patience and you should keep doing this until you are good at this important skill.
You might need some expert advice and support from your practice nurse or a children’s asthma nurse specialist to help you understand how to give the inhalers effectively.
Using inhalers correctly can mean the difference between your child’s asthma being well controlled so they can lead a normal life or being poorly controlled with frequent illness, time off school and distress.
The following film clips will show you the correct way to prepare, use and clean your child’s inhaler. This is important to get the correct dose of medicine from the inhaler.
To see a video of your inhaler select the image below.












If you do not see your inhaler on this list you can speak to your GP, nurse or pharmacist or check the patient information leaflet for your inhaler and medication.
Don’t forgot to return your inhalers to your local pharmacy where they can be safely disposed of or recycled, reducing waste and greenhouse gas emissions.
If your child has eczema or other conditions such as hayfever or allergic rhinitis which causes them to be hypersensitive, this can increase the likelihood that they will develop asthma.
Eczema, hayfever or allergic rhinitis, and other allergies can help support a diagnosis of asthma. If you notice any symptoms tell your GP or practice nurse.
Eczema is a skin condition which makes the child scratch as it is very itchy, uncomfortable and sometimes painful. When eczema is associated with an allergy it can be called atopic eczema. It can sometimes run in families.
Hay fever is caused by an allergic reaction to grass or tree pollens. It makes the child’s eyes red, watery and itchy. The hay fever season in the UK starts during the spring. Look out for symptoms from March to October. Symptoms are usually worse first thing in the morning and early evening, particularly on days that have been warm and sunny.
Allergic rhinitis makes the child have a runny nose as if they have a cold when they have been exposed to the substance they are allergic to. Children with perennial allergic rhinitis have symptoms all year round, and it can be easily mistaken for unusually persistent or frequent ‘colds’. Some children can develop sinusitis, where the cavities in the skull near to the cheek bones and eye brows become filled with fluid (they are normally filled with air) This causes pain and discomfort and occasionally infection. Nose bleeds can also be quite common with rhinitis. This is because the lining of the nose is itchy and is often rubbed or scratched.
Some children with asthma find their symptoms are worse in certain seasons.
Grass pollens, tree pollens and crops can all affect people triggering sneezing, and watery eyes in hayfever sufferers and further wheezing in children with asthma.
If your child has symptoms of allergy you should speak to your nurse, doctor or pharmacist to discuss the best antihistamine medicine for your child’s age and symptoms.
You can get daily information from the Met Office – air quality and Met Office – pollen count.
Night-time symptoms can be the worst to deal with for many. It can be hard to give asthma medicine or inhalers when your child is sleepy and you have just been woken up. These symptoms range from a persistent cough or wheeze when the child first lies down to sometimes happening in the middle of the night or first thing in the morning.
If this is becoming a struggle for you and your child speak to your GP, respiratory nurse or pharmacist. They may be able to give you alternatives or change a dose of medicine to fit in with your child’s night time routine.
See the topic on Sleep and asthma for more information.
If your child is regularly or frequently having asthma symptoms at night they should see your GP as soon as possible.

Children with asthma can become wheezy, breathless and have a cough triggered off by exercise, excitement and emotion.
This can lead to some children doing less or no physical exercise. Exercise is good for controlling asthma as long as your child has prepared by using inhalers before exercise and doing a gradual warm up. Many sportsmen and women have reached the top of their sport even though they have asthma.
Children with asthma should keep active and find a sport which suits them.
See the Exercise and sport for children with asthma section.
Symptoms are more likely if parents have asthma or some other condition (by which we mean eczema, hayfever and allergies).
This asthma connection is much stronger in parents, brothers and sisters than in more distant relatives.