GREEN AMBER! RED!!
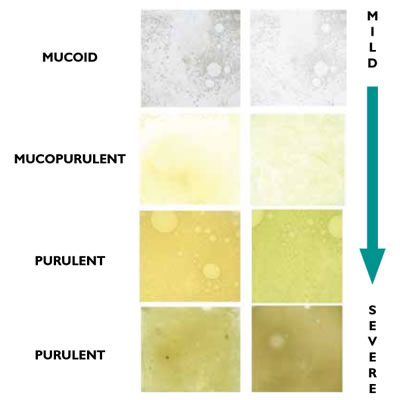
If you have COPD you are more likely to suffer from chest infections. Recognising the warning signs of infection is an important step in getting help quickly to reduce the impact before an infection can take hold. With every infection there is a risk that further damage will be done to the lungs.
It is important to know when an infection is beginning and get treatment from your GP as soon as possible.
A written plan to help you manage a chest infection can be presented as a set of ‘traffic lights’. Using the ‘traffic lights’ information will allow you to have a better understanding of your COPD and more control over your own health. ‘Traffic lights’ will alert you to when you should be contacting your GP or NHS 24 on 111 for advice and treatment.
Before using your local traffic lights system discuss with your doctor, respiratory nurse or healthcare professional. They will give you local contact details and information specific for you.