When you see the specialist, he or she will make a full assessment including:
- How you feel from day to day and what causes you problems (your symptoms).
- How far you can walk at a normal pace (to work out your breathlessness score – the MRC scale).
- Your inhaler technique should be checked to make sure you are using them correctly.
- If you have smoked – How much you have smoked.
- What jobs you have done in the past.
- Other health problems you have and treatment you are taking for these.
- A physical examination, to look for changes in your body from the normal which suggest COPD or other different diseases.
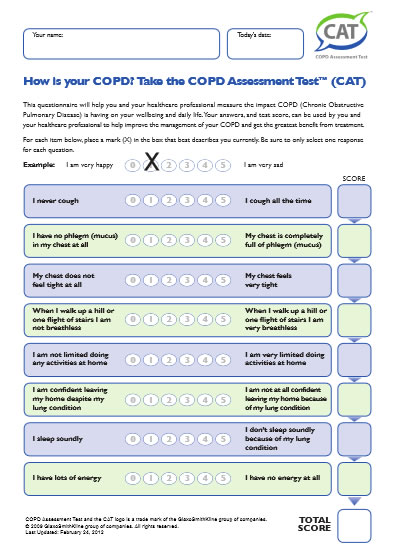
- You may be asked if COPD is affecting other aspects of your life such as your sleep, mood or how you are coping with daily tasks.