Please note there is no audio for this animation.
‘Cilia’ line your airways. These are tiny hairs forming brush-like structures. There are mucous producing cells in the larger airways known as goblet cells. This mucous may also be referred to as spit, phlegm or sputum. This mucous forms a moist layer on top of the cilia which helps to trap germs and small particles which are present in the air that you may have breathed in. The sweeping action of the brush-like cilia then carries this mucous, containing any germs and small particles to your mouth where it is either swallowed away into your stomach, or coughed up and spat out. This is the normal process for everyone.
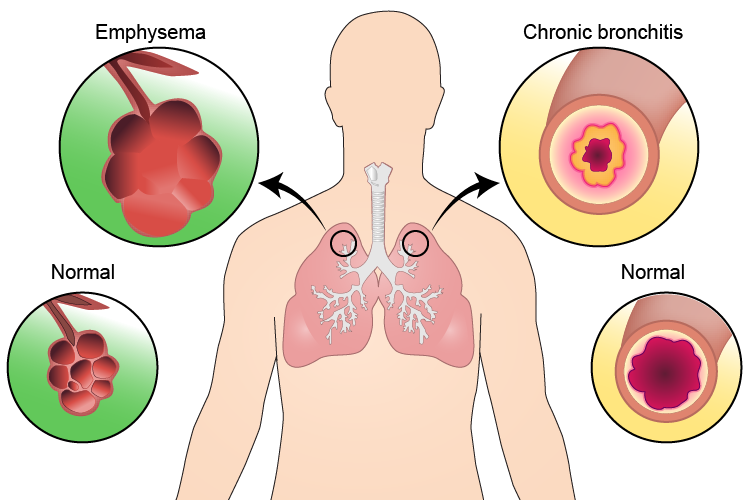
Some people with COPD may find it difficult to clear their airways, specialist physiotherapy techniques may help with this.